SAM-Competitive PRMT5 Inhibitor PF-06939999 Demonstrates Antitumor Activity in Splicing Dysregulated NSCLC with Decreased Liability of Drug Resistance.
Jensen-Pergakes, K., Tatlock, J., Maegley, K.A., McAlpine, I.J., McTigue, M., Xie, T., Dillon, C.P., Wang, Y., Yamazaki, S., Spiegel, N., Shi, M., Nemeth, A., Miller, N., Hendrickson, E., Lam, H., Sherrill, J., Chung, C.Y., McMillan, E.A., Bryant, S.K., Palde, P., Braganza, J., Brooun, A., Deng, Y.L., Goshtasbi, V., Kephart, S.E., Kumpf, R.A., Liu, W., Patman, R.L., Rui, E., Scales, S., Tran-Dube, M., Wang, F., Wythes, M., Paul, T.A.(2022) Mol Cancer Ther 21: 3-15
- PubMed: 34737197
- DOI: https://doi.org/10.1158/1535-7163.MCT-21-0620
- Primary Citation of Related Structures:
7MX7, 7MXA, 7MXC, 7MXG, 7MXN - PubMed Abstract:
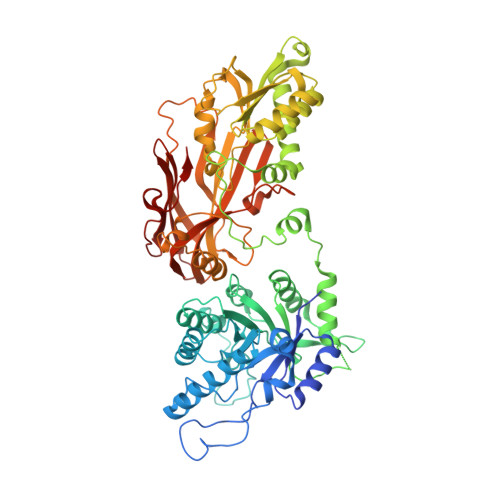
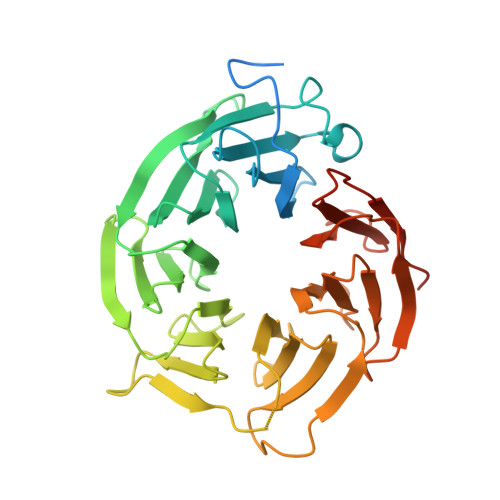
Protein arginine methyltransferase 5 (PRMT5) overexpression in hematologic and solid tumors methylates arginine residues on cellular proteins involved in important cancer functions including cell-cycle regulation, mRNA splicing, cell differentiation, cell signaling, and apoptosis. PRMT5 methyltransferase function has been linked with high rates of tumor cell proliferation and decreased overall survival, and PRMT5 inhibitors are currently being explored as an approach for targeting cancer-specific dependencies due to PRMT5 catalytic function. Here, we describe the discovery of potent and selective S-adenosylmethionine (SAM) competitive PRMT5 inhibitors, with in vitro and in vivo characterization of clinical candidate PF-06939999. Acquired resistance mechanisms were explored through the development of drug resistant cell lines. Our data highlight compound-specific resistance mutations in the PRMT5 enzyme that demonstrate structural constraints in the cofactor binding site that prevent emergence of complete resistance to SAM site inhibitors. PRMT5 inhibition by PF-06939999 treatment reduced proliferation of non-small cell lung cancer (NSCLC) cells, with dose-dependent decreases in symmetric dimethyl arginine (SDMA) levels and changes in alternative splicing of numerous pre-mRNAs. Drug sensitivity to PF-06939999 in NSCLC cells associates with cancer pathways including MYC, cell cycle and spliceosome, and with mutations in splicing factors such as RBM10. Translation of efficacy in mouse tumor xenograft models with splicing mutations provides rationale for therapeutic use of PF-06939999 in the treatment of splicing dysregulated NSCLC.
Organizational Affiliation:
Oncology Research Division, Pfizer Inc.; San Diego, California.